Introduction
Healthcare providers, insurance companies, and any entity handling sensitive patient data must understand the ins and outs of the Health Insurance Portability and Accountability Act (HIPAA) to ensure they’re maintaining the highest standards of data protection. But what does it mean when there’s a lapse in these standards? What are the repercussions when an organization or individual fails to adhere to HIPAA regulations?
The term ‘non-compliance with HIPAA’ is often thrown around, but its implications can be far-reaching and devastating for both patients and organizations involved. Non-compliance doesn’t just mean a mere oversight; it can entail a series of failures ranging from unauthorized data exposure to more egregious violations like selling patient information.
In this comprehensive guide, we will dissect the concept of non-compliance with HIPAA regulations to help you better understand the risks and ramifications. We will delve into the types of HIPAA violations, the scale of penalties that non-compliant entities might face, and actionable steps that can be taken to rectify and prevent such lapses.
Understanding non-compliance with HIPAA isn’t just a legal requirement; it’s a moral and ethical obligation to the people entrusting their most personal information to your care. With hefty fines, legal actions, and reputational damages at stake, ensuring compliance is not just advisable, it’s imperative.
So let’s venture into the complex world of HIPAA, unearthing what non-compliance really means, the risks that come with it, and the potentially dire consequences that healthcare organizations could face if they let their guard down.
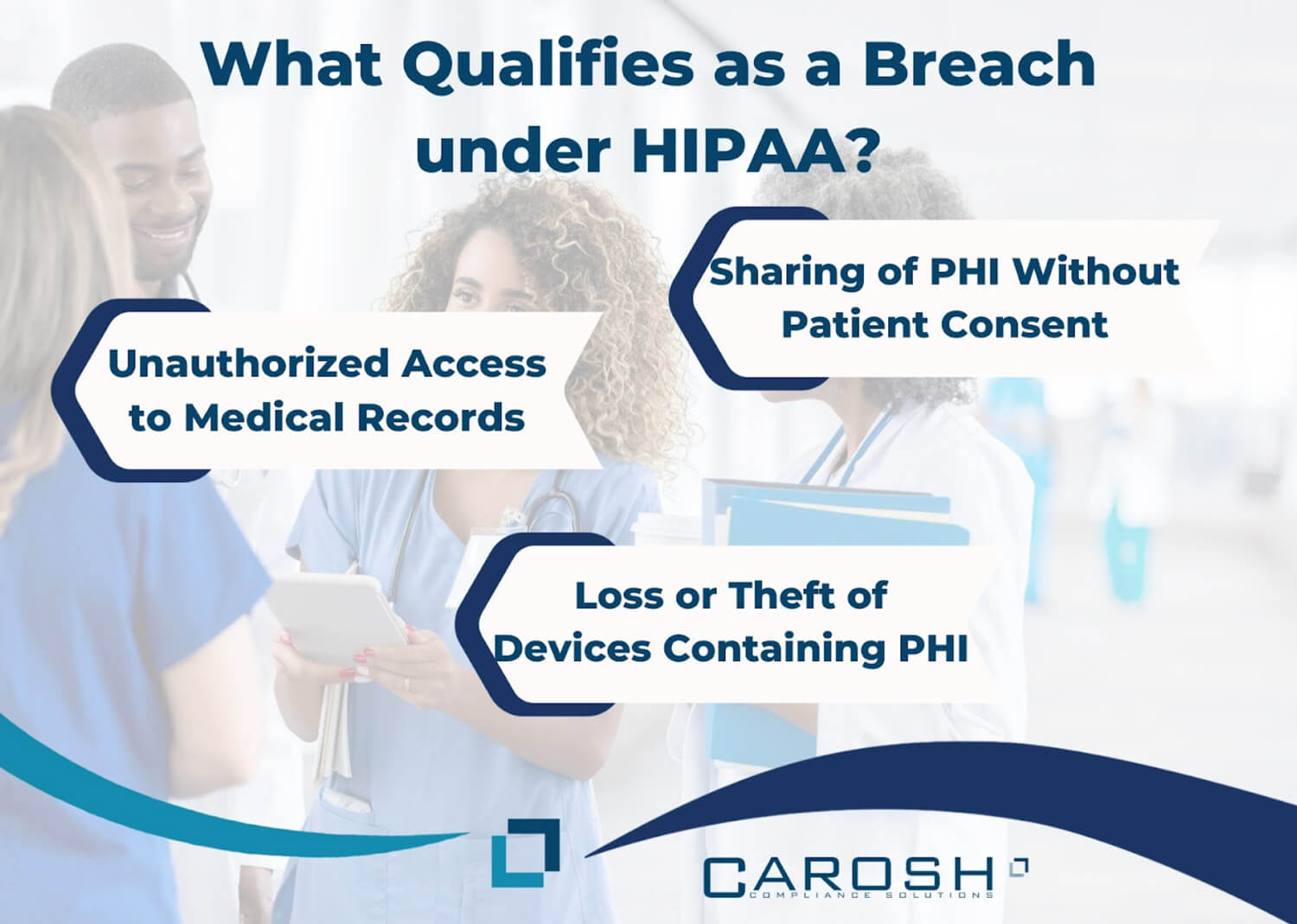
What Qualifies as a Breach under HIPAA?
Understanding what qualifies as a breach under the Health Insurance Portability and Accountability Act (HIPAA) is vital for any entity that handles or processes protected health information (PHI). A breach in this context refers to unauthorized access, use, or disclosure of PHI, which can happen in multiple ways. Below, we delve into meticulous details of some common forms of HIPAA breaches.
Unauthorized Access to Medical Records
When unauthorized individuals gain access to medical records, it’s considered a serious violation of HIPAA regulations. The perpetrators could be employees within the organization who do not have the requisite clearance, or external actors like hackers. Such access could result from:
- Weak Security Measures: Lack of robust security protocols, like strong passwords and multi-factor authentication, could make it easier for unauthorized individuals to gain access.
- Insider Misuse: Sometimes, staff members who aren’t authorized may access records out of curiosity, malice, or for personal gain.
- External Hacking: Cybercriminals could exploit vulnerabilities in the organization’s system to gain unauthorized access to medical records.
The risks are monumental, including identity theft, fraudulent insurance claims, and personal blackmail. Moreover, the healthcare organization risks incurring hefty fines, legal penalties, and reputational damage.
Sharing of PHI Without Patient Consent
The sharing of PHI without explicit consent from the patient is another critical form of a HIPAA breach. This can occur in various settings:
- Internal Sharing: An unauthorized staff member could share the PHI with other departments or individuals within the same organization for reasons not related to patient care.
- External Sharing: Sharing information with external organizations without patient consent, even if for research or reference purposes, is a breach.
- Online Leaks: Sometimes PHI might accidentally get posted online or sent in an unprotected email, becoming accessible to unauthorized individuals.
In all these cases, patient privacy is severely compromised, leading to potential misuse of sensitive information.
Loss or Theft of Devices Containing PHI
Loss or theft of laptops, smartphones, or any device containing PHI is a significant concern. If not encrypted or adequately secured, the information on these devices becomes ripe for unauthorized access. Here’s how this often happens:
- Physical Theft: Theft of computers or external hard drives from a secured area.
- Lost Devices: Loss of mobile devices or laptops in public places like cafes or airports.
- Unsecured Networks: Storing PHI on devices that are connected to unsecured networks, making them vulnerable to cyber theft.
Loss or theft not only leads to unauthorized access to PHI but also results in significant operational disruptions.
Exemptions
It’s important to note that not all unauthorized uses or disclosures constitute a breach. Exemptions might include accidental disclosures by a staff member who is authorized to access PHI, so long as the information isn’t further used or disclosed in a manner violating HIPAA. These accidental breaches must be immediately documented and reported, and corrective actions should be taken to prevent similar occurrences in the future.
By understanding these forms of breaches in-depth, healthcare organizations can take informed steps to strengthen their compliance measures, thereby better protecting the PHI they are entrusted with.
What is Considered “Unsecured Protected Health Information?”
The concept of “Unsecured Protected Health Information” (Unsecured PHI) is an important one in the context of HIPAA compliance. Simply put, PHI becomes “unsecured” when it is not adequately protected by certain technological or methodological safeguards mandated by the Secretary of Health and Human Services. Below are some meticulous details on what qualifies as “Unsecured PHI” and the different forms it can take.
Forms of PHI
Protected Health Information (PHI) exists in various formats, including:
- Electronic PHI (ePHI): Digital files, databases, electronic health records, etc.
- Verbal PHI: Oral communication between healthcare providers and staff.
- Physical PHI: Printed medical records, prescriptions, handwritten notes, etc.
Each of these forms can be “unsecured” if not adequately protected. To read more, click here.
Lack of Encryption
One of the most common ways PHI becomes unsecured is through the lack of encryption. In the case of ePHI, encryption transforms the original information into an unreadable format, which can only be reverted to a readable format by someone who has the cryptographic key. The absence of this layer of security in the storage, transmission, or sharing of ePHI makes the information unsecured.
- Data at Rest: ePHI stored in databases, hard drives, or any other storage medium must be encrypted.
- Data in Transit: ePHI sent over networks, whether internally within an organization or externally, must be encrypted to ensure that it is secure during transmission.
Inadequate Destruction Methods
When it comes to physical forms of PHI, shredding, pulping, or incinerating the information is essential for rendering it unreadable, indecipherable, and otherwise unable to be reconstructed. Failure to do so leaves the physical PHI “unsecured.”
- Paper Records: Simply discarding paper records into regular waste bins leaves them vulnerable to unauthorized access.
- Hardware: Physical storage media like external hard drives or servers should be destroyed or wiped clean of any retrievable PHI before disposal.
Insecure Verbal Communications
Even oral communications can be considered unsecured PHI if they’re inadequately protected. Conversations that occur in public areas where unauthorized individuals might overhear sensitive patient information are deemed unsecured.
- Public Places: Discussing PHI in hallways, elevators, or waiting rooms where unauthorized individuals may overhear.
- Insecure Phone Conversations: Discussing PHI over unsecured lines or in environments where the conversation can be overheard.
Policy and Training Gaps
Sometimes, unsecured PHI is not a result of technological failure but rather a failure in organizational policy or employee training.
- Lack of Training: Employees unaware of proper security measures may inadvertently leave PHI unsecured.
- Outdated Policies: Organizations with outdated or poorly implemented security policies may also be at risk of maintaining unsecured PHI.
Understanding what constitutes “Unsecured Protected Health Information” is crucial for healthcare entities to effectively implement safeguard measures. By paying attention to these specific aspects, organizations can better adhere to HIPAA regulations and mitigate the risk of unauthorized access or disclosure of PHI.
Timelines for Notifying Entities Post a Breach
Notify Affected Individuals Within 60 Days
The 60-day window for notifying affected individuals starts from the day the breach is discovered, not from the day the breach occurred. This is a crucial distinction. The notification should be sent via first-class mail unless an email consent has been given by the individual. This notification must be comprehensive, containing details such as what kind of data was breached, what steps are being taken to mitigate the impact, and what the affected individuals can do to protect themselves.
Notify the Secretary of Health and Human Services
The obligation to notify the Secretary of Health and Human Services (HHS) depends on the scale of the breach. For breaches affecting fewer than 500 individuals, healthcare providers can log this information and then submit all such small-scale breaches in a batch, annually. However, for breaches affecting 500 or more individuals, this notification to the Secretary must be made concurrently with the individual notifications, and without unreasonable delay.
Notify the Media if Over 500 Residents are Affected
If a breach affects more than 500 residents of a single state or jurisdiction, there is an additional requirement to notify a prominent media outlet in that state or jurisdiction. Like the notification to the Secretary, this should be done as soon as possible and not later than 60 days from the discovery of the breach. This is aimed at ensuring a wider reach of the information to possibly affected individuals.
Repercussions for Non-Compliance
Non-compliance with these notification requirements can result in significant penalties. These range from fines levied per violation to, in extreme cases, criminal charges. Penalties can vary based on the level of perceived negligence and can range from $100 to $50,000 per violation, with a maximum annual penalty of $1.5 million.
- Monetary Penalties: The Office for Civil Rights (OCR) can impose monetary fines, which are tiered based on the level of culpability. These fines can quickly add up if multiple instances of non-compliance are found.
- Civil Penalties: Civil action lawsuits can be taken against the healthcare provider, leading to financial burdens and reputational damage.
- Criminal Charges: Willful neglect that results in unauthorized disclosure can lead to criminal charges and imprisonment for responsible individuals.
- Regulatory Action: Beyond fines, entities may face regulatory action, which can include the loss of the ability to bill Medicare or Medicaid, or even the revocation of the license to operate.
- Reputational Damage: The reputation of the healthcare provider can take a significant hit, leading to loss of clientele, which in the long run can be financially debilitating.
Understanding the timelines and repercussions can help organizations prepare better and act swiftly in case of a breach, potentially reducing the scale of damage and associated penalties. To read more, click here.
How to Avoid Non-Compliance
Regularly Update Security Measures
- Software Updates and Patches: Keeping all software up-to-date is a basic but critical component of cybersecurity. Regularly apply patches and updates to all systems that access or store PHI.
- Firewalls and Intrusion Detection Systems: Employ robust firewalls to prevent unauthorized access and set up intrusion detection systems to alert you of any potential unauthorized entry into your network.
- Encryption: Use strong encryption protocols for data both in transit and at rest. This makes it significantly harder for malicious actors to interpret any data they might access.
- Multi-Factor Authentication: Require multiple forms of verification before granting access to PHI, as this adds an additional layer of security.
Train Staff on HIPAA Compliance
- Initial Training: All staff members should receive HIPAA training as part of their orientation. The training should cover the basic tenets of HIPAA, the importance of PHI, and the consequences of non-compliance.
- Ongoing Training: Regular refreshers and updates are critical as HIPAA regulations can change. At least annually, or more often if there are regulatory changes, staff should receive updated training.
- Role-Based Access: Training should also be specific to the roles of the individuals. Not everyone in a healthcare organization needs access to all PHI.
- Real-World Scenarios: Utilize real-world scenarios during training sessions to help staff better understand how to handle various situations.
Perform Risk Assessments
- Annual Reviews: At least once a year, an internal or third-party assessment of your compliance status should be conducted.
- After Changes: Whenever there’s a major change to your IT systems, another risk assessment should be conducted.
- Identify Risks: Go beyond technological risks to include human risks, environmental factors, and operational procedures.
- Remediation Plans: After identifying vulnerabilities, develop a remediation plan to address them and ensure that corrective actions are taken. Carosh Compliance Solutions can help create and implement remediation plans, to get more information on Carosh’s services, see here.
Conclusion
Avoiding non-compliance with HIPAA is a continuous process that involves both technological and human elements. Through rigorous, updated security measures, comprehensive training for staff, and regular risk assessments, healthcare organizations can make strong strides toward safeguarding the sensitive information they handle. Not only does this protect the organization from the severe penalties of non-compliance, but it also serves to protect the wellbeing and privacy of the patients they serve.