As medical professionals and healthcare organizations, the importance of adhering to the Health Insurance Portability and Accountability Act (HIPAA) cannot be overstated. HIPAA sets the standard for protecting sensitive patient data, and any failure to comply with its regulations can lead to substantial fines.
Understanding the Penalties
In 2023, HIPAA violation penalties continue to underscore the gravity of protecting patient information. The fines have been recalibrated, taking into account the cost of living adjustments, ensuring that the penalties maintain their deterrent effect despite economic changes.
The enforcement of these penalties is a dual effort. The OCR, a federal body, is the primary enforcer, tasked with overseeing compliance and acting against breaches. State attorneys general also play a critical role, particularly in instances where state privacy laws may impose stiffer penalties. They have the authority to pursue actions against covered entities and business associates under HIPAA, although this power is infrequently exercised, with most preferring to leverage state laws.
Civil penalties vary, depending on the degree of negligence. They range from violations made despite reasonable efforts to prevent them, to outright willful neglect. Criminal penalties are reserved for more severe violations, such as those committed with intent or due to willful neglect that is not corrected in a timely manner.
The OCR and state attorneys general aim not just to penalize but also to correct and improve privacy practices. Settlements often include a corrective action plan to address deficiencies in compliance, with the goal of strengthening the privacy and security of health information systems.
The updated penalty structure and the continued diligence of enforcement agencies serve as a potent reminder of the importance of HIPAA compliance. For healthcare providers, staying abreast of these regulations and understanding the potential financial implications of non-compliance is essential. It underscores a proactive approach to patient data protection, which is a cornerstone of the healthcare industry’s commitment to patient privacy and trust.
The Updated Civil Monetary Penalties
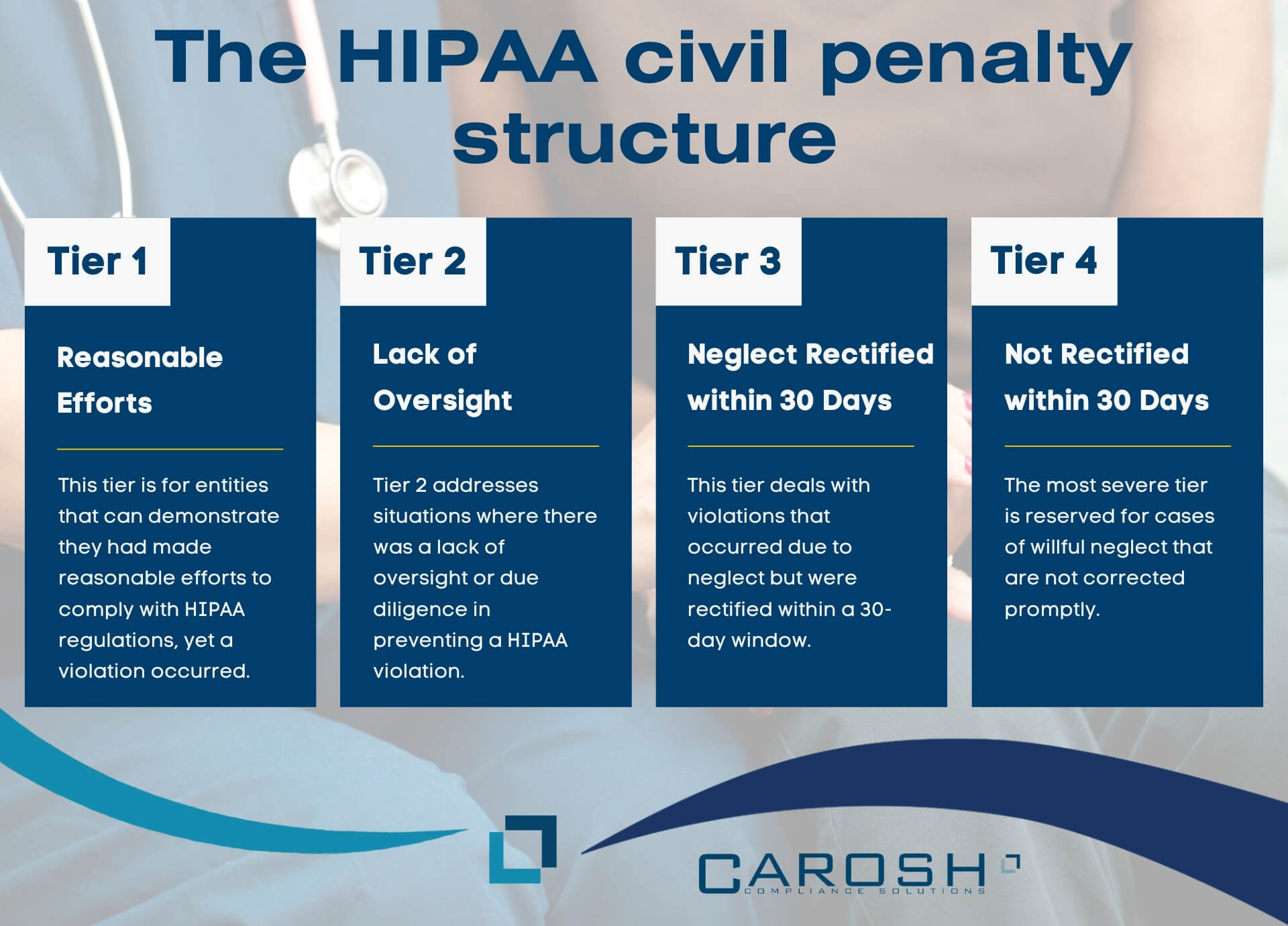
The HIPAA civil penalty structure is a nuanced system designed to match the severity of the violation with an appropriate sanction, reflecting the level of culpability involved in the breach of patient data privacy.
Tier 1: Reasonable Efforts
This tier is for entities that can demonstrate they had made reasonable efforts to comply with HIPAA regulations, yet a violation occurred. Back in the day fines started at a modest $137, acknowledging the attempts to comply, now published fines start at around $25,000 but can rapidly escalate to $68,928 for each violation, reflecting that compliance efforts must be thorough and ongoing. The annual limit for these violations is over $2 million, which serves as a substantial deterrent against complacency in maintaining patient data security.
Tier 2: Lack of Oversight
Tier 2 addresses situations where there was a lack of oversight or due diligence in preventing a HIPAA violation. The starting fine of $1,379 signifies that more could have been done to prevent the breach, while the upper limit matches Tier 1, emphasizing that the failure to oversee and manage HIPAA obligations is as serious as the violation itself. The annual cap being the same as Tier 1 reinforces that sustained oversight is expected to prevent repeated violations.
Tier 3: Neglect Rectified within 30 Days
This tier deals with violations that occurred due to neglect but were rectified within a 30-day window. The fines began at $13,785, recognizing the negligence but also acknowledging the swift action to rectify the situation. However, penalties can reach up to $68,928 per violation, underlining the serious nature of neglect when it comes to patient privacy.
Tier 4: Neglect Not Rectified within 30 Days
The most severe tier is reserved for cases of willful neglect that are not corrected promptly. Each violation carries a heavy fine of $68,928, with no lower limit, indicating a zero-tolerance policy for prolonged neglect. The annual limit of $2,067,813 is a clear message that immediate action is expected when a violation is identified.
The OCR notice in 2019 further refines these tiers by imposing specific annual caps that differ from the per-violation fines. This discrepancy acknowledges that while a single violation might attract a significant penalty, the overall annual financial burden for an entity that has multiple violations in a year is capped at a lower level to allow for the possibility of recovery and correction. This approach balances the need to punish non-compliance and the desire to not financially cripple healthcare entities, thus maintaining their ability to provide care.
State Fines
At the state level, the authority vested in state attorneys general allows them to enforce HIPAA regulations by imposing fines that can be substantial. The cap of $25,000 per violation category each year is indicative of the serious stance states take on the protection of health information. Furthermore, this cap is not static; it is adjusted annually to account for inflation, ensuring that the fines retain their weight in real terms over time.
State attorneys general have the discretion to pursue penalties under state privacy laws, which may sometimes prescribe harsher penalties than federal HIPAA regulations. This dual layer of potential financial repercussions—state and federal—serves as a powerful deterrent and a reminder of the importance of compliance.
The choice to pursue state laws often comes down to the practicality and potential severity of penalties. If state laws allow for stronger penalties or if the process to litigate under these laws is more streamlined, state attorneys general may opt for this route. This strategic use of state laws underscores the complex legal landscape within which HIPAA-covered entities must operate.
The presence of these state-level fines also highlights the importance for healthcare entities to not only be conversant with federal HIPAA regulations but also to be well-informed about state laws that govern patient health information. Compliance programs within healthcare organizations must therefore be comprehensive, taking into account the variegated tapestry of regulations that span from the federal to the state level.
Recent Settlements as Cautionary Tales
The settlements in 2023 underscore the significant consequences of non-compliance with HIPAA regulations. They serve as cautionary tales, emphasizing the real-world implications of failing to adequately protect patient information.
Settlements for HIPAA violations are not mere punitive measures; they are reflective of the broader need to maintain public trust in healthcare systems. When a healthcare provider or associated business fails to perform sufficient risk analyses, it leaves patient data vulnerable to breaches, which can have far-reaching implications for individuals’ privacy and the integrity of healthcare services.
Similarly, impermissible disclosures of PHI represent a serious breach of patient trust and confidentiality. The legal settlements for such disclosures signal to all healthcare entities the importance of stringent data controls and the need to educate employees on the proper handling of sensitive information.
Lastly, the HIPAA Right of Access is a critical patient right that has been enforced strictly. Settlements related to breaches of this right highlight the necessity for healthcare providers to ensure timely and appropriate access to patient records.
The range of settlements—from tens of thousands to over a million dollars—reflects the varying degrees of severity and the scale of the breaches. Healthcare entities are reminded through these financial penalties that compliance is not just a legal obligation but a core aspect of patient care. These cases illustrate the importance of ongoing diligence and the need for robust compliance programs that can adapt to evolving threats and regulatory expectations.
Staying Compliant
Staying compliant with HIPAA regulations is an ongoing process that requires healthcare entities to be proactive and vigilant. Regular risk analyses are fundamental, allowing entities to identify and mitigate potential vulnerabilities in their systems. This involves a thorough examination of all aspects of how patient data is handled, stored, and transmitted.
Reviewing system activity records is another critical component, providing oversight and ensuring that all access to PHI is appropriate and authorized. This also helps in detecting and responding to potential security incidents promptly.
Aligning policies and procedures with the HIPAA Security Rule is not a one-time task; it requires continuous review and updates to adapt to new threats, technological advances, and changes in healthcare practices. Healthcare entities must ensure that their workforce is adequately trained and that their practices are both effective and current.
Furthermore, when a compliance failure occurs, it is often not enough to simply pay a fine. Corrective action plans are commonly mandated, requiring entities to implement specific measures to prevent future violations. These plans typically involve a combination of administrative, technical, and physical safeguards tailored to the specific shortcomings identified during the investigation of the breach.
Overall, compliance is a dynamic challenge that demands a strategic approach, integrating risk management, staff training, and policy development to create a robust culture of privacy and security within healthcare organizations.
A Final Word
The evolution of healthcare, marked by rapid technological advancements, has made HIPAA compliance an increasingly complex endeavor. With the digitization of medical records, telemedicine, and the integration of AI into patient care, healthcare providers must navigate a labyrinth of new privacy challenges. However, the essence of HIPAA compliance transcends these complexities—it’s about safeguarding patient trust. This trust is the bedrock upon which the provider-patient relationship is built and is critical for the delivery of high-quality healthcare.
To maintain this trust, healthcare entities must be proactive in their approach to compliance. For help with staying compliant and proactive, click here. This means staying informed about the latest regulatory changes, investing in robust security infrastructure, and fostering a culture where patient privacy is a paramount concern. Regular training, clear communication, and a commitment to ethical practices are essential.
As the healthcare landscape continues to shift, those who prioritize patient privacy and make concerted efforts to comply with HIPAA will not only avoid financial penalties but also solidify their reputation as trustworthy stewards of personal health information. In this ever-evolving field, vigilance and commitment to privacy are not just regulatory requirements but are integral to the noble endeavor of providing care.
In conclusion, HIPAA compliance in 2023 remains a critical obligation for healthcare entities, underscored by a structured penalty system that imposes significant fines for violations. With penalties adjusted for inflation and categorized into tiers based on culpability, the stakes for maintaining patient privacy are high. State-level fines add another layer of accountability, emphasizing the importance of adherence to both federal and state regulations. Recent settlements highlight the costly consequences of non-compliance, serving as cautionary examples for all healthcare providers. As the healthcare landscape evolves, maintaining compliance is not just about avoiding fines but also about upholding the essential trust between patients and providers.




